Polycystic Ovary Syndrome (PCOS) is a complex and common hormonal disorder that affects females. It is characterized by a range of symptoms and can lead to various related health conditions. PCOS is estimated to affect 1 in 10 individuals of reproductive age, making it one of the most prevalent endocrine disorders in women. This article aims to provide a comprehensive overview of PCOS and its associated conditions, including its causes, symptoms, diagnosis, and treatment options.
Polycystic Ovary Syndrome is a multifactorial condition that involves hormonal imbalances and metabolic disturbances. It is typically diagnosed based on the presence of at least two of the following criteria:
Irregular menstrual cycles: PCOS often manifests as irregular or absent periods due to disrupted ovulation.
Elevated levels of androgens: Increased levels of male hormones, such as testosterone, can lead to symptoms like acne, hirsutism (excessive hair growth), and male-pattern baldness. And
Polycystic ovaries: On ultrasound imaging, the ovaries may appear enlarged and may contain multiple small cyst-like structures.
Causes and Risk Factors
While, the exact cause of PCOS is still not fully understood, it is believed to result from a combination of genetic, environmental, and hormonal factors. Some common risk factors associated with PCOS include:
Genetics: A family history of PCOS can increase the likelihood of developing the condition.
Insulin Resistance: Insulin resistance is often present in individuals with PCOS, leading to elevated insulin levels and contributing to the hormonal imbalances seen in the condition.
Hormonal Imbalances: Increased levels of luteinizing hormone (LH) and reduced levels of follicle-stimulating hormone (FSH) can disrupt ovulation and contribute to PCOS symptoms.
Obesity: Excess body weight, especially abdominal fat, can exacerbate PCOS symptoms and increase the risk of associated conditions.
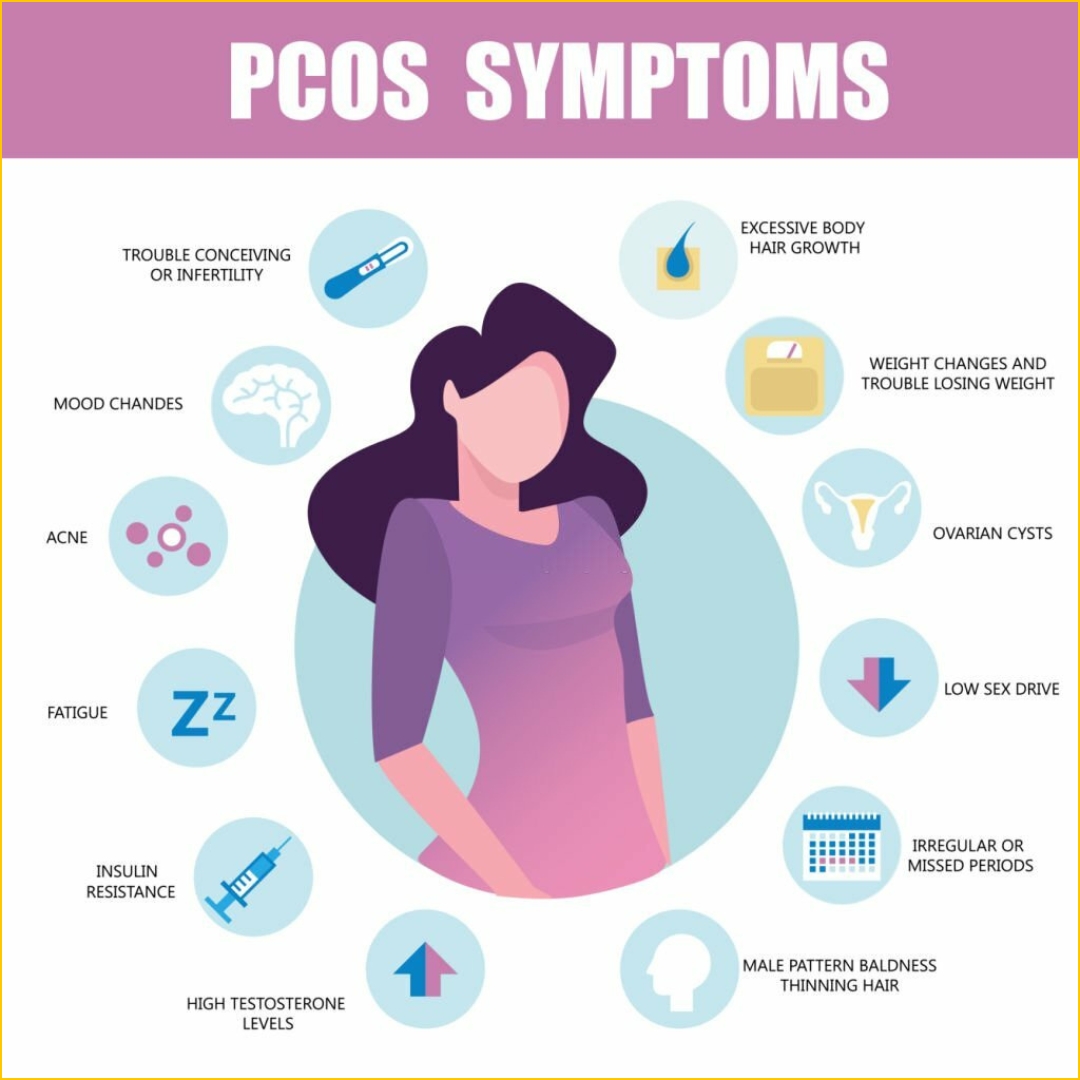
Symptoms of PCOS
The symptoms of PCOS can vary widely from person to person, and not all individuals with PCOS will experience the same set of symptoms. Common symptoms include:
Irregular Menstrual Periods: The hallmark of PCOS is irregular or absent menstrual cycles due to disrupted ovulation.
Hirsutism: Excessive hair growth in areas such as the face, chest, back, and abdomen can be a distressing symptom for many individuals with PCOS.
Acne and Oily Skin: Elevated androgen levels can lead to acne and increased oil production in the skin.
Hair Loss: Some individuals with PCOS may experience male-pattern baldness or thinning hair.
Weight Gain and Obesity: PCOS is often associated with weight gain and obesity, which can worsen hormonal imbalances and metabolic issues.
Insulin Resistance: Many individuals with PCOS have insulin resistance, which can lead to higher blood sugar levels and an increased risk of type 2 diabetes.
Mood Disorders: PCOS has been linked to an increased risk of depression and anxiety.
Fertility Issues: Ovulatory dysfunction can make it challenging for individuals with PCOS to conceive.
If you suspect you have PCOS or are experiencing symptoms, it is crucial to consult with a gynecologist for a proper evaluation and personalized treatment plan
PCOS and Associated Health Conditions
Polycystic Ovary Syndrome is not limited to its reproductive symptoms. It can also lead to various related health conditions, which are essential to recognize and manage. Some of these include:
Type 2 Diabetes
Insulin resistance is a common feature of PCOS, and over time, it can lead to the development of type 2 diabetes. Regular monitoring of blood glucose levels and lifestyle modifications are crucial in managing this risk.
Cardiovascular Disease
PCOS is associated with an increased risk of cardiovascular disease. Factors such as obesity, high blood pressure, and abnormal lipid profiles contribute to this elevated risk. Lifestyle changes and, in some cases, medication may be needed to mitigate these risks.
Endometrial Hyperplasia and Cancer
Irregular or absent menstrual cycles can lead to endometrial hyperplasia, a condition in which the lining of the uterus becomes thickened. This can increase the risk of endometrial cancer in individuals with PCOS. Regular gynaecological screenings are essential for early detection and prevention.
Sleep Apnea
Obesity, a common comorbidity in PCOS, increases the risk of sleep apnoea. This condition can have serious health consequences and should be evaluated and treated by a healthcare professional.
High Blood Pressure (Hypertension)
Obesity and insulin resistance in PCOS can contribute to high blood pressure, which, if left untreated, can increase the risk of cardiovascular events such as heart attacks and strokes.
Non-Alcoholic Fatty Liver Disease (NAFLD)
Insulin resistance and obesity can also lead to the accumulation of fat in the liver, a condition known as non-alcoholic fatty liver disease. NAFLD can progress to more severe liver conditions if not managed properly.
Psychological and Emotional Health
PCOS can have a significant impact on psychological and emotional well-being. The hormonal fluctuations, body image concerns, and fertility struggles associated with PCOS can contribute to anxiety and depression. Seeking support and counselling can be vital for mental health.
Diagnosis of PCOS
Diagnosing PCOS involves a thorough evaluation by a healthcare provider, which may include:
Medical History: A detailed medical history, including menstrual patterns, symptoms, and family history, is essential for diagnosis.
Physical Examination: A physical examination may reveal signs of hirsutism, acne, or other PCOS-related symptoms.
Blood Tests: Blood tests are used to measure hormone levels, including testosterone, LH, FSH, and insulin. Elevated levels of these hormones can help confirm the diagnosis.
Ultrasound Imaging: Transvaginal ultrasound can reveal the presence of polycystic ovaries and assess the thickness of the endometrial lining.
Glucose Tolerance Test: This test assesses insulin resistance and can help determine the risk of type 2 diabetes.
Lipid Profile: Lipid profiles measure cholesterol and triglyceride levels, important for assessing cardiovascular risk.
Treatment Options for PCOS
The management of PCOS and its associated conditions often involves a multifaceted approach that addresses both the hormonal and metabolic aspects of the condition. Treatment options include:
Lifestyle Modifications
Weight Management: Achieving and maintaining a healthy weight through diet and exercise is a cornerstone of PCOS management, as it can improve insulin sensitivity and reduce the severity of symptoms.
Diet: A balanced diet that focuses on whole foods, fibre, and controlled carbohydrate intake can help manage insulin resistance and support weight loss.
Exercise: Regular physical activity, including both cardiovascular and strength training exercises, can help improve insulin sensitivity and aid in weight management.
Polycystic Ovary Syndrome is a complex hormonal disorder that affects multiple aspects of an individual's health. Recognizing the signs and symptoms of PCOS is essential for early diagnosis and intervention. Effective management strategies encompass lifestyle modifications, medication when necessary, and emotional support. Regular monitoring and collaboration with healthcare professionals can help individuals with PCOS lead healthier lives and reduce the risk of associated conditions such as type 2 diabetes, cardiovascular disease, and endometrial cancer. Ultimately, raising awareness and understanding of PCOS is crucial to improving the quality of life for those affected by this common hormonal disorder.
If you suspect you have PCOS or are experiencing symptoms, it is crucial to consult with a gynecologist for a proper evaluation and personalized treatment plan
Related Blog Articles
1. PCOS and Its Related Conditions
2. Infertility in Men and Women
3. Endometriosis: The Hidden Cause of Irregular Periods
.webp)