Cervical cancer is a significant health concern for women worldwide, but unfortunately, misinformation and myths surrounding this disease persist. Dispelling these myths is crucial for raising awareness, promoting early detection, and ultimately saving lives. In this blog post, we'll debunk some of the most prevalent myths about cervical cancer and provide accurate information to empower women to take charge of their health.
Myths and Facts about Cervical Cancer
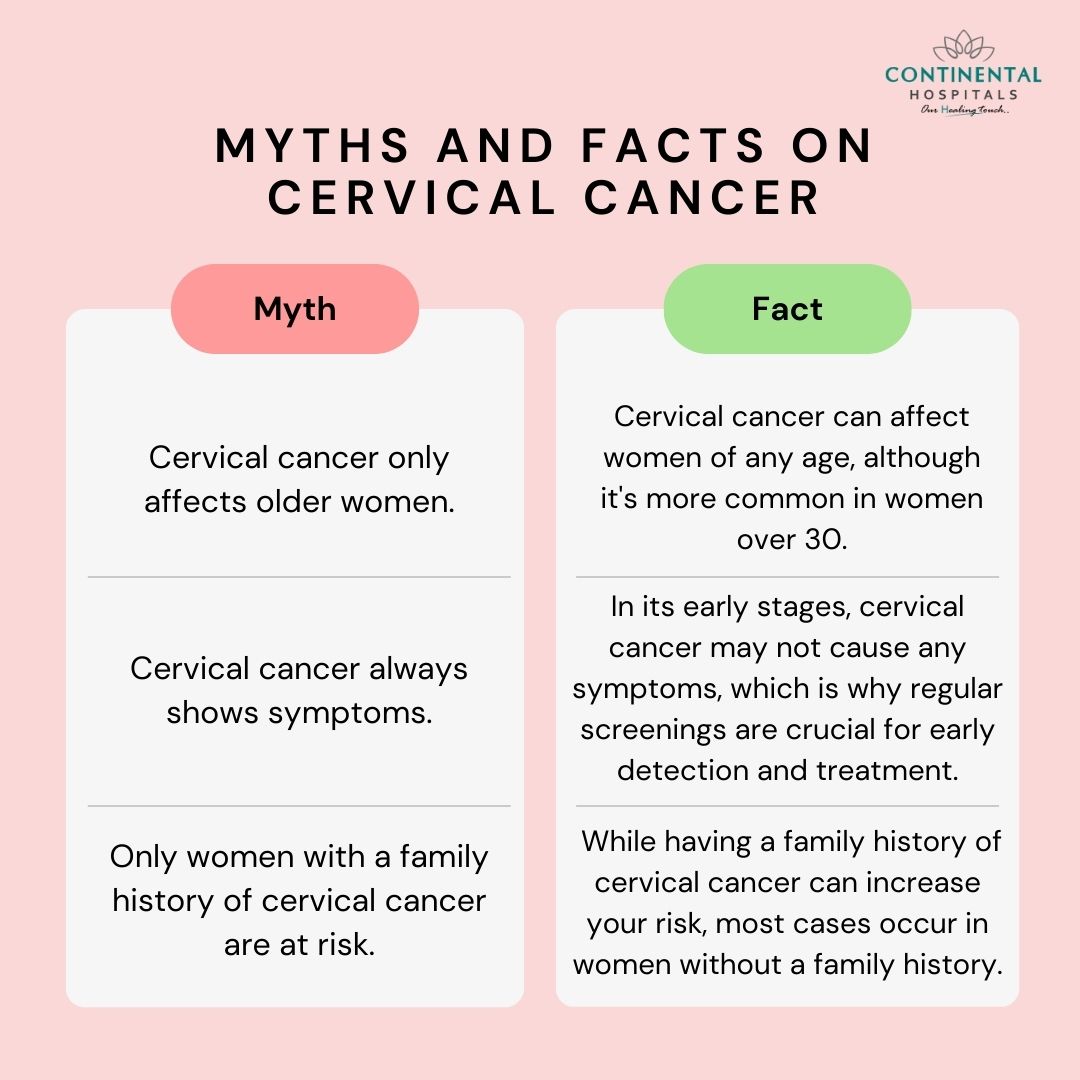
Myth 1: Cervical cancer only affects older women.
Fact: While cervical cancer is more common in older women, it can affect women of any age. Younger women can also develop cervical cancer, especially if they have been exposed to risk factors such as human papillomavirus (HPV) infection or if they have a weakened immune system. Women of all ages need to attend regular cervical cancer screenings to detect any abnormalities early.
Myth 2: HPV vaccination provides complete protection against cervical cancer.
Fact: While HPV vaccination significantly reduces the risk of developing cervical cancer, it does not provide complete protection. There are several strains of HPV, and the vaccines currently available target the most common ones associated with cervical cancer. However, vaccination does not eliminate the risk, so regular screening for cervical cancer remains important for early detection and treatment.
Myth 3: Cervical cancer is always hereditary.
Fact: While some cases of cervical cancer may have a hereditary component, the majority are caused by the human papillomavirus (HPV). HPV is a sexually transmitted infection, and certain high-risk strains of the virus can lead to the development of cervical cancer. Other risk factors for cervical cancer include smoking, a weakened immune system, multiple sexual partners, and a history of sexually transmitted infections.
Myth 4: Cervical cancer is not preventable.
Fact: Cervical cancer is highly preventable through vaccination against HPV, regular cervical cancer screenings (such as Pap smears or HPV tests), and practicing safe sex. HPV vaccination can significantly reduce the risk of developing cervical cancer by protecting against the most common cancer-causing strains of the virus. Screening tests can detect abnormal cervical cells early, allowing for prompt treatment before cancer develops or progresses.
Myth 5: Cervical cancer always presents symptoms.
Fact: In its early stages, cervical cancer often does not cause any symptoms, which is why regular screening is crucial for early detection. As the cancer progresses, symptoms may include abnormal vaginal bleeding (such as between periods, after sex, or after menopause), pelvic pain, pain during sex, and unusual vaginal discharge. However, these symptoms can also be caused by conditions other than cervical cancer, so it's important to consult a healthcare provider for proper evaluation.
Myth 6: Only women who have had multiple sexual partners are at risk of cervical cancer.
Fact: While having multiple sexual partners does increase the risk of exposure to HPV, the primary cause of cervical cancer, it is not the only risk factor. Any woman who has ever been sexually active is at risk of HPV infection and consequently, cervical cancer. Other risk factors include smoking, a weakened immune system, early sexual activity, and a history of sexually transmitted infections.
Myth 7: Cervical cancer is always fatal.
Fact: Cervical cancer is highly treatable, especially when detected early through regular screening. The survival rate for cervical cancer varies depending on the stage at diagnosis and the effectiveness of treatment. Early-stage cervical cancer often has a very high survival rate, with many women being cured of the disease. Advances in treatment options, including surgery, radiation therapy, chemotherapy, and targeted therapies, have improved outcomes for women diagnosed with cervical cancer.
Myth 8: Cervical cancer is contagious.
Fact: Cervical cancer itself is not contagious, but the human papillomavirus (HPV) that is responsible for most cases of cervical cancer is a sexually transmitted infection. HPV can be transmitted through skin-to-skin contact, including sexual activity. However, not everyone infected with HPV will develop cervical cancer, and the virus can also be cleared by the immune system in many cases. Practicing safe sex and getting vaccinated against HPV can reduce the risk of HPV transmission and cervical cancer.
Myth 9: Cervical cancer screenings are painful and invasive.
Fact: Cervical cancer screenings, such as Pap smears and HPV tests, are generally quick, simple, and relatively painless procedures. During a Pap smear, a healthcare provider gently collects cells from the cervix using a small brush or spatula, which may cause mild discomfort but is not typically painful. HPV tests involve similarly collecting a sample of cells. While some women may experience slight discomfort during these screenings, the benefits of early detection far outweigh any temporary discomfort.
Myth 10: Cervical cancer only affects women.
Fact: While cervical cancer predominantly affects women, HPV infection, which is the primary cause of cervical cancer, can also lead to other types of cancer in both men and women. These include cancers of the anus, penis, vagina, vulva, and oropharynx (the back of the throat, including the base of the tongue and tonsils). HPV vaccination is recommended for both males and females to reduce the risk of HPV-related cancers in both sexes.
Dispelling myths about cervical cancer is essential for promoting awareness, early detection, and prevention. By understanding the facts and taking proactive steps such as regular screenings, HPV vaccination, and adopting a healthy lifestyle, women can reduce their risk of cervical cancer and lead healthier lives. It's crucial to empower women with accurate information so they can make informed decisions about their health and well-being.
If you have concerns about your cervical cancer, it's best to consult with a Cancer specialist who can assess your risk factors.
Related Blog Topics:
1. HPV Vaccine: A powerful tool in preventing Cervical Cancer
2. Indian Government Initiative in Promoting Cervical Vaccines
.webp)