Frequently Asked Questions
Kwashiorkor is a type of severe malnutrition characterized by a deficiency of protein in the diet. It often occurs in children, particularly in areas where there is a lack of access to a balanced and nutritious diet.
The primary cause of Kwashiorkor is insufficient protein intake, often in combination with a diet lacking essential nutrients. It is prevalent in regions where there is limited access to protein-rich foods.
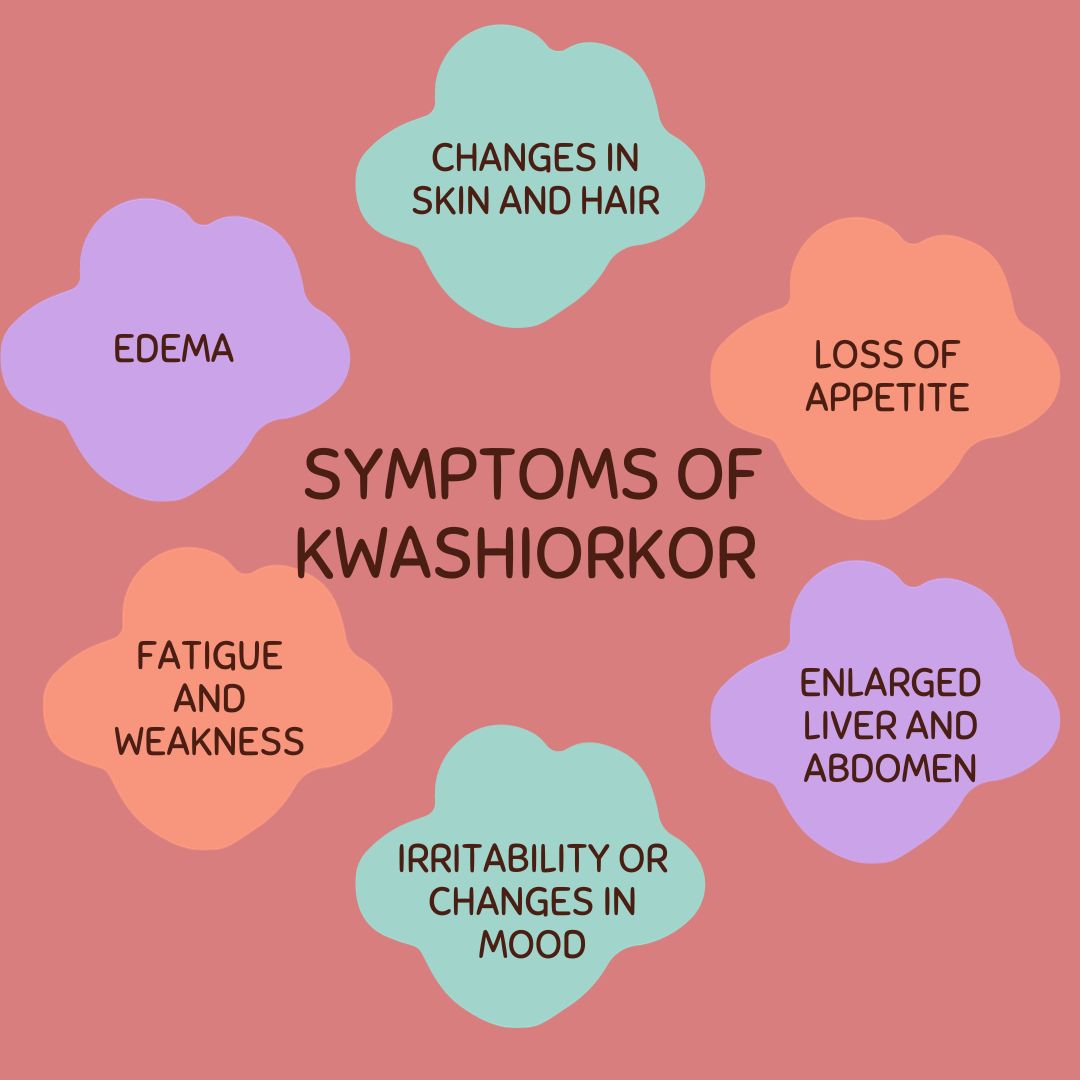
Symptoms of Kwashiorkor include swelling (edema), particularly in the legs and feet, along with a distended belly. Other signs may include skin changes, hair discoloration, fatigue, irritability, and a failure to grow or gain weight.
Diagnosis is typically based on clinical signs and symptoms, such as edema and nutritional deficiencies. Laboratory tests may also be conducted to assess protein levels and other nutritional markers.
Yes, Kwashiorkor can be treated with a well-balanced and nutritious diet that includes sufficient protein, calories, vitamins, and minerals. In severe cases, hospitalization may be necessary to provide specialized care.
Kwashiorkor is more prevalent in developing countries where there is a lack of access to adequate nutrition. It can occur in regions facing food shortages, poverty, and inadequate healthcare.
Yes, Kwashiorkor can be prevented by ensuring access to a balanced and nutritious diet that includes sufficient protein, vitamins, and minerals. Public health measures, education, and support for vulnerable populations are crucial for prevention.
While Kwashiorkor is most commonly associated with children, severe malnutrition can affect individuals of any age. However, children are particularly vulnerable due to their rapid growth and development.
If treated promptly and effectively, the majority of children with Kwashiorkor can recover without significant long-term consequences. However, in severe cases or if left untreated, Kwashiorkor can lead to lasting developmental and health issues.
Individuals can contribute to the prevention of Kwashiorkor by supporting organizations that work on improving nutrition in vulnerable communities, raising awareness about the importance of balanced diets, and advocating for policies that address food insecurity and poverty.
.webp)


 040 6700 0000
040 6700 0000  040 6700 0111
040 6700 0111